My anatomy teachers taught me that the primary purpose of the Ilio Tibial Band (ITB) was to provide lateral stabilization. However, recent research, including studies from Catherine Eng, summarized in the Harvard Gazette, tells a different story.
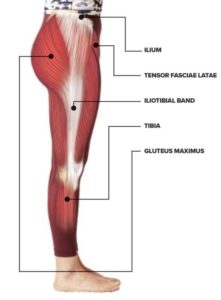 The ITB connects the Gluteus Maximus (GMax) and the Tensor Fascia Latae (TFL) to the lower leg (tibialis anterior and tibia). This large piece of fascia originates from the outside of the buttock, the crest of the hip (ileum) and the outside of the upper thigh and runs down the outside of the leg, attaching below the knee. The ITB is a long, flat tendon. It may well have a role in stability – tests with cadavers have shown that tremendous machine-generated forces only lengthen the ITB by just 1-2mm!
The ITB connects the Gluteus Maximus (GMax) and the Tensor Fascia Latae (TFL) to the lower leg (tibialis anterior and tibia). This large piece of fascia originates from the outside of the buttock, the crest of the hip (ileum) and the outside of the upper thigh and runs down the outside of the leg, attaching below the knee. The ITB is a long, flat tendon. It may well have a role in stability – tests with cadavers have shown that tremendous machine-generated forces only lengthen the ITB by just 1-2mm!
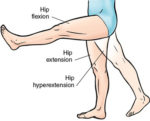
Eng explains that the front part of the ITB stretches as the leg swings backward, storing elastic energy. That stored energy is released as the leg swings forward during a stride, returning energy. The back portion of the ITB stretches as the leg swings forward and returns energy as the leg extends backward. These dynamic stretches are driven by movement and make substantial changes to the tissue over time.
 In athletes, the shortened ITB can rub over the femoral condyle outside the knee (or sometimes near the hip), inflaming the ITB. Typically, we trigger this by over-training and other training errors. Some pain may come from tension on the upper and lower attachments of the ITB itself. Anatomical differences make some people more likely to develop ITB inflammation.
In athletes, the shortened ITB can rub over the femoral condyle outside the knee (or sometimes near the hip), inflaming the ITB. Typically, we trigger this by over-training and other training errors. Some pain may come from tension on the upper and lower attachments of the ITB itself. Anatomical differences make some people more likely to develop ITB inflammation.
Different considerations apply to the general, less athletic population. Imagine a 58-year-old woman who has not exercised much over the years and has become less flexible. She began walking regularly and has developed signs of ITB. Chances are that her gait has shortened; her leg doesn’t go into significant extension or flexion at the hip anymore.
Consequently, the rear part of the ITB is not stretching dynamically as her leg swings forward, and the front part isn’t stretching as the leg swings backward. For her, a shortened gait translates into a shortened ITB that can rub across the femoral epicondyle and become irritated – just as for the over-training athlete.
Increasing the stride will dynamically stretch and gradually lengthen the ITB, reducing inflammation. Given the strength of the ITB, you cannot lengthen the ITB with any static stretches.
Self Care Treatment
Before these gentle, passive stretches, trigger points in the muscles should be cleared with self-compression using a tennis ball or other tool. Listed below are muscles often contributing to ITB pain or a shortened stride. It isn’t an exhaustive list, but it is helpful as a starting point.
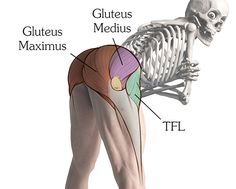
TFL stretch – TFL tensions the rear section of the ITB; we want movement here.

Gluteus maximus – Provides dynamic stretch on the front of the ITB as the leg extends.

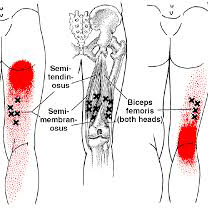
Hamstring stretch – Tight hamstrings are the primary limitation of the leg swinging forward.

Rectus Femoris stretch – This is the only quad that crosses the hip and can restrict hip extension.

Gluteus medius – Stabilizes the hip and assists in properly moving the TFL.


Spinal erector stretch – Often recruited by weak glutes to assist with extension of the thigh at the hip.

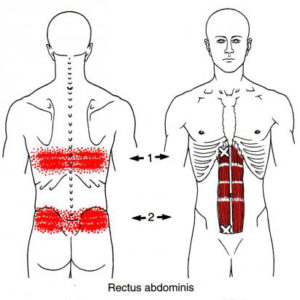
Rectus abdominis stretch – The superficial abs become tight, hindering full leg extension.

Transversus Abdominis –Reduces static load on the spinal erectors and glutes.

Success in any specific stretch is less critical than lengthening the stride overall. Some may find that pain or other limitations in their knees, hips and low back limit their ability to perform this entire routine comfortably. If so, modify as needed.
We want to stretch the front and back aspects of the IT band AND strengthen the muscles that will help maintain that stretch as you walk with a longer and stronger stride.
If you think you are having IT band pain, you may find that a session or two to identify and treat the root causes of your case is helpful.
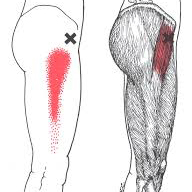
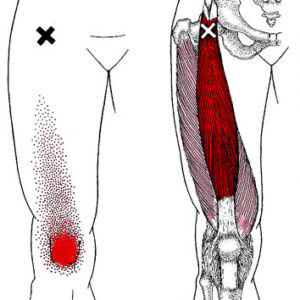
Trigger Point Activations in TFL and Glutes
 Trigger points in the TFL usually result from sudden overload or regularly walking or running on a surface sloped to one side. A sloped running surface reduces pronation on one side and increases it on the other (see article on Shin Splints and other Tibialis Anterior problems).
Trigger points in the TFL usually result from sudden overload or regularly walking or running on a surface sloped to one side. A sloped running surface reduces pronation on one side and increases it on the other (see article on Shin Splints and other Tibialis Anterior problems).
Slanted surfaces also causes one leg to bow slightly at the knee (genu varus) and the other to bend in (genu valgus). Running up and down hills can also overload the TFL, especially if your foot already pronates due to a shortened first metatarsal.
In runners, an inadequate warmup routine or poor conditioning can lead to muscle injuries that cause or perpetuate trigger points in the TFL.
You can activate trigger points in any muscle by keeping the muscle shortened for a long time; for instance, by sleeping in the fetal position or sitting with the knees above the hips.
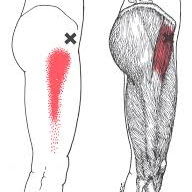
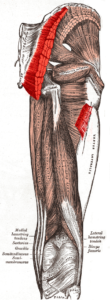
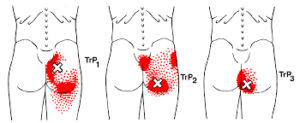
The pain of tensor fascia latae trigger points is very similar to TrPs from the gluteus minimus, gluteus medius and vastus lateralis muscles. Trigger points from the quadratus lumborum can also refer to the hip.
Trigger points in the TFL can occur in isolation. Still, more frequently, they develop with TrPs in the anterior gluteus minimus and the related rectus femoris, iliopsoas, or sartorius muscles.
In particular, active TrPs in the gluteus minimus must be released to allow the complete range of motion needed for trigger points in the TFL to release.
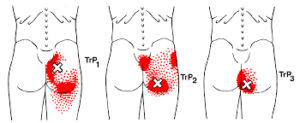
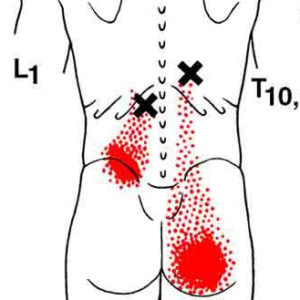
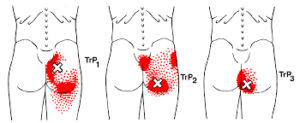 Trigger points in the gluteus maximus can refer pain and other symptoms to the sacrum and tailbone area, the lower buttock and the upper, outside area near the hip.
Unlike the radiating referrals of the other glutes, TrPs in the gluteus maximus tends to remain local.
You may experience pain when sitting if you have gluteus maximus trigger points, trying to avoid pressure or lean to the opposite side. You may squirm in your seat to prevent discomfort.
Gluteus maximus TrPs can also cause pain when walking, especially uphill. The forward lean of your trunk can overload the gluteus maximus. These symptoms can be similar to sacroiliac inflammation.
Pain from TrPs in this muscle intensifies with vigorous contractions of a muscle that is already shortened—for instance, kicking while swimming can cause this, especially in cold water.
The explosive starts typical of tennis, beach volleyball, or sprints can overload your gluteus maximus, resulting in symptoms similar to an upper hamstring strain.
Trigger points in the gluteus maximus can refer pain and other symptoms to the sacrum and tailbone area, the lower buttock and the upper, outside area near the hip.
Unlike the radiating referrals of the other glutes, TrPs in the gluteus maximus tends to remain local.
You may experience pain when sitting if you have gluteus maximus trigger points, trying to avoid pressure or lean to the opposite side. You may squirm in your seat to prevent discomfort.
Gluteus maximus TrPs can also cause pain when walking, especially uphill. The forward lean of your trunk can overload the gluteus maximus. These symptoms can be similar to sacroiliac inflammation.
Pain from TrPs in this muscle intensifies with vigorous contractions of a muscle that is already shortened—for instance, kicking while swimming can cause this, especially in cold water.
The explosive starts typical of tennis, beach volleyball, or sprints can overload your gluteus maximus, resulting in symptoms similar to an upper hamstring strain.
 Associated trigger points can develop in the referral zone of a primary TrP. This can be because the muscle is related as a functional synergist or antagonist or because the muscles share innervation or proximity.
Associated trigger points can develop in the referral zone of a primary TrP. This can be because the muscle is related as a functional synergist or antagonist or because the muscles share innervation or proximity.
 For example, muscles in the referred pain zone of gluteus maximus include: piriformis, gluteus medius, gluteus minimus, quadratus lumborum, obturators, gemelli, coccygeus, adductor magnus and proximal hamstrings.
For example, muscles in the referred pain zone of gluteus maximus include: piriformis, gluteus medius, gluteus minimus, quadratus lumborum, obturators, gemelli, coccygeus, adductor magnus and proximal hamstrings.
 There are other muscles that refer pain into the buttock that should also be assessed. It is possible that the gluteus maximus TrP is actually secondary. These include iliocostalis lumborum, rectus abdominis, pelvic floor and soleus.
There are other muscles that refer pain into the buttock that should also be assessed. It is possible that the gluteus maximus TrP is actually secondary. These include iliocostalis lumborum, rectus abdominis, pelvic floor and soleus.
 A strong antagonist like iliopsoas may require treatment. If full extension of the hip is limited due tightness of the psoas, releasing those TrPs may restore enough range of motion to fully treate the gluteus maximus trigger points.
A strong antagonist like iliopsoas may require treatment. If full extension of the hip is limited due tightness of the psoas, releasing those TrPs may restore enough range of motion to fully treate the gluteus maximus trigger points.
Extra – Function and Anatomy of TFL and Glutes
Structure
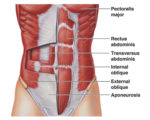
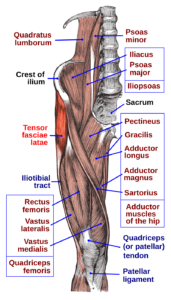 It arises from the anterior part of the outer lip of the iliac crest; from the outer surface of the anterior superior iliac spine, and part of the outer border of the notch below it, between the gluteus medius and sartorius; and from the deep surface of the fascia lata.
It is inserted between the two layers of the iliotibial tract of the fascia lata about the junction of the middle and upper thirds of the thigh. The tensor fasciae latae tautens the iliotibial tract and braces the knee, especially when the opposite foot is lifted. The terminal insertion point lies as far as the lateral condyle of the tibia.
It arises from the anterior part of the outer lip of the iliac crest; from the outer surface of the anterior superior iliac spine, and part of the outer border of the notch below it, between the gluteus medius and sartorius; and from the deep surface of the fascia lata.
It is inserted between the two layers of the iliotibial tract of the fascia lata about the junction of the middle and upper thirds of the thigh. The tensor fasciae latae tautens the iliotibial tract and braces the knee, especially when the opposite foot is lifted. The terminal insertion point lies as far as the lateral condyle of the tibia.
Nerve supply
Tensor fasciae latae is innervated by the superior gluteal nerve, L5 and S1. At its origins of the anterior rami of L4, L5, and S1 nerves, the superior gluteal nerve exits the pelvis via greater sciatic foramen superior to the piriformis. The nerve also courses between the gluteus medius and minimus. The superior gluteal artery also supplies the tensor fasciae latae.[1] The superior gluteal nerve arises from the sacral plexus and only has muscular innervation associated with it. There is no cutaneous innervation for sensation that stems from the superior gluteal nerve.[2]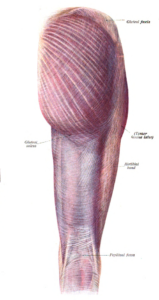 The gluteus maximus (also known collectively with the gluteus medius and minimus, and sometimes referred to informally as the "glutes") is the main extensor muscle of the hip. It is the largest and exterior-most of the three gluteal muscles and makes up a large portion of the shape and appearance of each side of the hips. Its thick fleshy mass, in a quadrilateral shape, forms the prominence of the buttocks. Its average weight of 844g is more than twice that of the other glutes together and it often measures 2.5cm (1 inch) thick.
The gluteus maximus (also known collectively with the gluteus medius and minimus, and sometimes referred to informally as the "glutes") is the main extensor muscle of the hip. It is the largest and exterior-most of the three gluteal muscles and makes up a large portion of the shape and appearance of each side of the hips. Its thick fleshy mass, in a quadrilateral shape, forms the prominence of the buttocks. Its average weight of 844g is more than twice that of the other glutes together and it often measures 2.5cm (1 inch) thick.
Organization
The gluteus maximus is larger and more extensive in humans than any other primate. In adapting to bipedal gait, reorganization of the attachment of the muscle as well as the moment arm was required. Some of these evolutionary changes include shortening and tilting of the pelvis to permit extension of the thigh, a more horizontal angulation of the muscle and significant enlargement compared to other primates. This structure supports the upright posture and and bipedal walking of humans. Humans are the only mammal that can place the center of mass of our head, arms and torso over our hips. The evolutionary change presumably freed our hands for other activities are believed to be crucial to the development of manual dexterity and intelligence in humans. The muscle is remarkably coarse in function and structure, made up of muscle fascicles lying parallel with one another, and collected together into larger fibrous bundles.Structure
 It arises from the posterior gluteal line of the inner upper pelvic bone, and roughly the portion of the bone including the crest of the hip bone, immediately above and behind it; and from the posterior surface of the lower part of the sacrum, the base of the spine, and the side of the coccyx, the tailbone; from the aponeurosis of the erector spinae (lumbodorsal fascia), the sacrotuberous ligament, and the fascia covering the gluteus medius (gluteal aponeurosis). The fibers are directed obliquely downward and lateralward; The gluteus maximus has two insertions:
It arises from the posterior gluteal line of the inner upper pelvic bone, and roughly the portion of the bone including the crest of the hip bone, immediately above and behind it; and from the posterior surface of the lower part of the sacrum, the base of the spine, and the side of the coccyx, the tailbone; from the aponeurosis of the erector spinae (lumbodorsal fascia), the sacrotuberous ligament, and the fascia covering the gluteus medius (gluteal aponeurosis). The fibers are directed obliquely downward and lateralward; The gluteus maximus has two insertions:
- those forming the upper and larger portion of the muscle, together with the superficial fibers of the lower portion, end in a thick tendinous lamina, which passes across the greater trochanter, and inserts into the iliotibial band of the fascia lata;
- the deeper fibers of the lower portion of the muscle are inserted into the gluteal tuberosity between the vastus lateralis and adductor magnus.
Consider These Changes
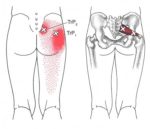
 Trigger points in the TFL can be caused by sudden trauma, such as landing on from high jump. More often if comes from chronic overload, such as jogging up and down hill without support for a pronated foot.
In general, extended walking or running on uneven surfaces can activate tensor fascia latae TrPs because they force one foot into pronation and the other into supination and have a compensatory effect on your knees and hips.
Poor conditioning and inadequate warmups can lead to injuries that activate or perpetuate TrPs in the TFL muscle. Weakness or inhibition of the gluteus medius or gluteus minimus can cause overload of the TFL because they act together to stabilize the hip.
As with other muscles, the tensor fascia latae are aggravated by immobilization in the shortened position for extended periods of time. For example, this happens during prolonged sitting or sleeping on your side with your hips tightly flexed. Walking with heavy loads can also overload this muscle.
Trigger points in the TFL can be caused by sudden trauma, such as landing on from high jump. More often if comes from chronic overload, such as jogging up and down hill without support for a pronated foot.
In general, extended walking or running on uneven surfaces can activate tensor fascia latae TrPs because they force one foot into pronation and the other into supination and have a compensatory effect on your knees and hips.
Poor conditioning and inadequate warmups can lead to injuries that activate or perpetuate TrPs in the TFL muscle. Weakness or inhibition of the gluteus medius or gluteus minimus can cause overload of the TFL because they act together to stabilize the hip.
As with other muscles, the tensor fascia latae are aggravated by immobilization in the shortened position for extended periods of time. For example, this happens during prolonged sitting or sleeping on your side with your hips tightly flexed. Walking with heavy loads can also overload this muscle.
 Pain in the buttocks can also be caused by lumbar disc and facet pathologies, sacroiliac joint dysfunction, coccynynia or hip joint problems.
However, some diagnosed with trochanteric bursitis, including those treated successfully with a local anesthetic, actually have gluteus maximus TrPs that area.
You can perform self-pressure release with a Backknobber, a lacrosse ball or tennis ball. If your glutes are very sensitive, you may even need to start with a larger fitness ball. If you can, try holding up your weight to moderate the pressure between the floor and your glutes. If you find it more comfortable, you can apply the same technique against a wall.
Hold pressure for 15-25 seconds, repeating for up to six repetitions. This can be done as up to every two to three hours, as long as your symptoms are still being relieved. Be cautious not to use too much pressure. This can activate or perpetuate trigger points.
If you have gluteus maximus TrPs you should avoid prolonged sitting. If you work with a computer, you should request an ergnonomic assessment and modifications to your workstation.
It is best to have a desk that is adjustable between standing and sitting, with a chair to match. It should also have adjustable arm rests and lumbar supports. Pay special attention to the fabric and padding of the seat. Move frequently!
Side sleeping with the painful side up and a thick pillow between your knees can reduce symptoms and improve sleep quality.
Pain in the buttocks can also be caused by lumbar disc and facet pathologies, sacroiliac joint dysfunction, coccynynia or hip joint problems.
However, some diagnosed with trochanteric bursitis, including those treated successfully with a local anesthetic, actually have gluteus maximus TrPs that area.
You can perform self-pressure release with a Backknobber, a lacrosse ball or tennis ball. If your glutes are very sensitive, you may even need to start with a larger fitness ball. If you can, try holding up your weight to moderate the pressure between the floor and your glutes. If you find it more comfortable, you can apply the same technique against a wall.
Hold pressure for 15-25 seconds, repeating for up to six repetitions. This can be done as up to every two to three hours, as long as your symptoms are still being relieved. Be cautious not to use too much pressure. This can activate or perpetuate trigger points.
If you have gluteus maximus TrPs you should avoid prolonged sitting. If you work with a computer, you should request an ergnonomic assessment and modifications to your workstation.
It is best to have a desk that is adjustable between standing and sitting, with a chair to match. It should also have adjustable arm rests and lumbar supports. Pay special attention to the fabric and padding of the seat. Move frequently!
Side sleeping with the painful side up and a thick pillow between your knees can reduce symptoms and improve sleep quality.
