As a myofascial therapist, I know that chronic headache pain is routinely listed as the second most common chronic pain complaint after back pain. If we grouped it with neck and shoulder pain, it would certainly be #1.
However, I want to focus on classic headache pain. After all, it is a complicated topic on its own, so we will have our hands full.
This is an introduction to chronic headache pain and myofascial therapy approaches to treating it.
They have been around the block, so to speak, and have often endured a variety of treatments. Unfortunately, many of these are not effective.
In addition, many people are motivated to reduce or eliminate the medications that are almost inevitable. Whether you regularly take Excedrin when a headache crops up or are taking poweful drugs for migraines and other severe headaches, you may want to stop that medication. Of course, we know that we need to attempt that gradually.
In addition, many people are motivated to reduce or eliminate the medications that are almost inevitable. Whether you regularly take Excedrin when a headache crops up or are taking poweful drugs for migraines and other severe headaches, you may also want to stop that medication. Of course, we know that we need to consult our physician and reduce medications gradually.
Causes of Chronic Headaches
Most sufferers have had a variety of tests searching for a causative diagnosis. We are sorting out options for chronic headache pain myofascial treatment. Therefore, we assume that most of these alternative diagnoses have been eliminated. For instance, we assume that you do not currently have a brain tumor, a slow-bleeding sub-dural hematoma, Chiari malformation, etc.
All of these medical diagnoses for headache, and more, require proper evaluation and treatment by an appropriate MD or OD.
Myofascial Therapy Can Be Very Helpful
However, even in these cases, myofascial pain can be part of the picture. Complete resolution may require myofascial therapy to fully resolve chronic headache pain.
Finally, if we assume you are suffering from a true migraine, cluster headache, or certain other types, you are probably being treated with medication and/or other means.
Yes, we all hope you can move past those treatments. However, this may take some time. At first, we like to think of chronic headache pain myofascial therapy as another important tool in your kit to manage chronic headaches!

Myofascial Aspects of Chronic Headache Pain
Is This You?
Unfortunately, you have classic, one-sided migraine without aura. Yours is triggered by MSG and certain scents. Light is intolerable and no OTC medication is effective. Your hand on the same side is typically cold.
Myofascial treatment is an important aspect of comprehensive migraine treatment.
Subsequently, you have had a series of tests that don’t reveal too much. However, your doctor thinks that there may be a problem with blood vessels in your brain. She prescribed some medication to help, but you can only take it a few times a month.
In addition, you received some nifty bio-feedback training. In learning how to warm your hands, your migraines relent. Of course, you also avoid your triggers, like MSG and perfumes.
Fortunately, you are much improved, but not completely better. Why?
Myofascial pain can be one of the peripheral system stimulants that causes a fully developed migraine. Release some of these muscles is helpful.
In addition, some of these muscular problems can restrict venous return from the brain and cause it to back up. In turn, blood pressure within the vessels in the brain can increase. Some of these can also interfere with blood supply to your arm, making your hand colder.
Addressing muscle imbalance issues is necessary to eliminate a key myofascial perpetuating factor.
Maybe with chronic headache pain – myofascial treatment of these muscles will also help!
Tension headache is a broad term that can include some forms of cervicogenic headache (originating in your neck) and other types related to stress, posture, exertion, etc. Most tension headaches have significant myofascial components.
Is This You?
You have dull, aching head pain. It still feels pretty severe to you. It feels like there is a band around your head. Sometime it is tight across your forehead. However, sometimes you feel it along the sides and back of your head. In addition, your scalp, neck and shoulder muscles are usually tender when you have a headache.
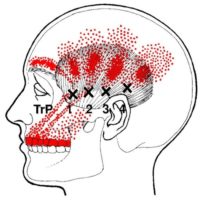
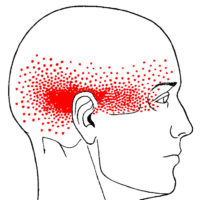
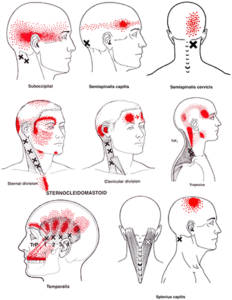
Many of the common pain patterns of tension headache match almost precisely some common myofascial referral patterns in the head.
Episodic tension headaches
Your husband gets tension headaches too, but they only last an hour or two. Maybe even a couple of days if it is really bad. But he doesn’t get them that often. Your headaches started that way, but then they became chronic. But your husband just takes some OTC meds if he needs to, once and a while, and he’s fine.
Chronic tension headaches
However, your headaches last longer. Sometimes, it seems like they never go away! You have then at least half the time and its been going on this way for many months.
Your friend who has migraines says she thinks you have migraines too. Your symptoms are kind of similar. Sometimes, you wonder if you have both kinds of headaches. Some people can have both!
But unlike your friend, you don’t have visual disturbances, nausea or vomiting when you have a tension headache. Physical activity makes your friend’s migraine worse. But your tension headache pain don’t seem to be affected by your workouts. Sometimes you are sensitive to bright light and loud sounds but nothing like your friend! It’s like she has a bad hangover on migraine days…
Cervicogenic headache it is accompanied by neck pain and stiffness. Also, certain neck movements can provoke cervicogenic headaches. According to the NIH headache classification this is the third, discrete primary headache type after migraine and tension headache.1
Is This You?
However, sometimes you feel it one side of your head. Often, it settles right behind one eye.. In addition, you have have:
- pain and stiffness of the neck
- pain around the eyes
- sensitivity to light and noise
- nausea
- blurred vision
That sounds quite a bit like a migraine or a tension headache! Except that, cervicogenic headaches usually include these symptoms too:
- Reduced range of motion in the neck
- Pain in the neck, shoulder, or arm on one side
- Head pain that is triggered by certain neck movements or positions
Many of the common pain patterns of cervicogenic headache match almost precisely some common myofascial referral patterns in the head.
Is This You?
You happen to be a male in your your 40’s, you still smoke more than you’d like to admit and drink socially. Your buddy told you that one of those ED drugs has really enhanced things with his partner and he gave you a couple. You figured, “Why not?” and gave it a try.
Cluster Headaches Often Start Suddenly
THEN, you got one of those horrible headaches again! You’ve had cluster headaches before – literally clusters of headaches that last for for weeks, sometimes even a month! The last time was over a year ago but based on experience you know what you are in for. Your sister gets them sometimes too.
Excruciating pain usually starts in, behind or around one of your eyes, but then radiates to other areas of your face, head and neck. Your eye is watering and with a droopy eyelid. Just like last time!
Traditional Treatment For Cluster Headaches
You’ve been given some prescription nasal sprays but your’re not sure about them. One time you had to go the the ER and got some IV triptan medication that worked.
Your doctor also prescribed some steroids and even lithium as a preventative. But, it has been such a long time you haven’t taken anything in months.
Myofascial Treatment Options
Eventually, these awful headaches will pass. However, in the meantime, are there any muscles that contribute to this pain? Do any of the headache referral patterns look familiar?
Maybe treating some of these muscles will also help!
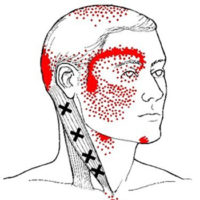
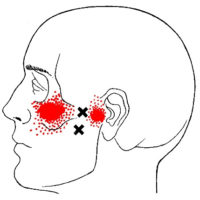
The SCM and upper trapezius referral patterns look a lot like cluster headache pain.
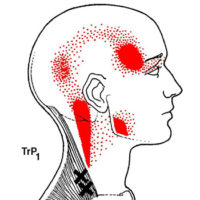
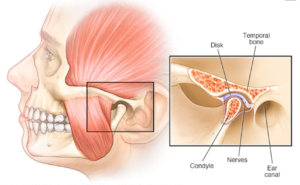
If you have a TMJ Headache – Myofascial Pain should be on your radar! Problems with the Temporo-Mandibular Joint (TMJ) cause pain in the face and head. In addition, TMJ disorders (TMJD) can cause myofascial problems AND myofascial dysfunction can cause TMJ pain, reinforcing each other.
Sometimes, TMJ headache – myofascial pain also feeds tension and migraine headaches.
The pterygoid referral patterns are closely related to TMJ headache pain.

For instance, sinus headaches are typically related to sinus infections. Chronic sinus infections should be treated first. Subsequently, if myofascial problems remain, they can be treated next.
Headaches due to trauma present a different challenge. An acute condition can quickly become chronic. Treatment of headache associated with whiplash is topic in its own right.
Similarly, treatment of traumatic brain injury (TBI) is often a multi-disciplinary process. Myofascial therapy can be a part of that treatment but does not address TBI directly.
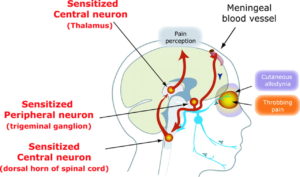
Allodynia
Allodynia occurs when you experience pain from things that are normally not painful. For example, simple touch or pressure become painful. Nerves in the area that was touched sends signals to your brain. But, your nervous system is in a heightened state. So, your brain doesn't produce a mild sensation of touch as it should. Instead, it produces a sensation of pain and discomfort.Hyperalgesia
Hyperalgesia occurs when something that typically painful is more painful than it should be. For example, a simple bump would ordinarily be mildly painful. However, if you are a chronic pain patient it might send your through the roof. Again, your nervous system is more sensitive. Of course, it produces pain that is amplified.Other Symptoms of Central Sensitization
Central sensitivity has other characteristics. They occur less often. For example, it can lead to heightened sensitivities across all your senses. For instance, some chronic pain patients report sensitivities to light, sounds and odors. Normal levels of light can seem too bright. Perfume can produce a headache... In addition, central sensitivity is associated with cognitive deficits. For instance, this includes poor concentration and poor short-term memory. Also, it corresponds with increased levels of emotional distress, particularly anxiety. After all, the nervous system isn't just responsible for sensations, like pain. In addition, it produces our emotions. Central sensitivity can occur with chronic low back pain, chronic neck pain, whiplash injuries, headaches and other conditions.Fortunately, for Chronic Pain - Myofascial Trigger Point Therapy helps break the cycle of central sensitivity...
Chronic Headache and Myofascial Therapy
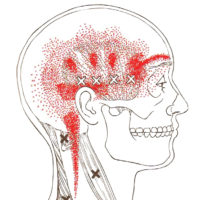
First stop to consider where your own pain is. We will usually have you draw it. Pay more attention to the location and how it radiates than how good your art skills are. Knowing the location accurately is important. You might need someone else to look at where you say it hurts other than where you draw it. We often have especially poor visualization of where our our pain is on the back side of the torso.
Where Does The Pain Refer?
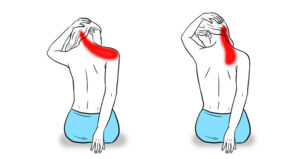
Next, we take a look at referral patterns for that part of the body. These usually show an outline of the muscle with a referral pattern, typically in red, spread over that muscle and extending around it.
Sometimes, there is more than one referral pattern that seems to match your pain. In that case, we’re going to need to look more closely at some other aspects of these muscles.

The manual compressions of trigger point therapy are not simply deep tissue massage. A well trained trigger point therapist knows exactly where the trigger points for these muscles are supposed to be. We also know that there are lots of variations and we know how to feel the difference. Finally, the actual technique that we use to apply trigger point pressure release is not as simple as pushing hard on a given spot. We work into it gradually and more deeply than traditional massage therapy does.
Why Do We Focus on Manual Pressure Release?
There are other ways to treat trigger points, but manual pressure release has been documented to be as effective as dry needling and more effective than cupping and most other techniques. It is completely non-invasive and safe when practiced by a skilled therapist.
Fascial Stretching
Fascial stretching is a gentle technique for balancing the length of connective tissues by working together with you to gradually move connective tissues. We can’t actually make significant changes to your connective tissue with just our hands.
If we could easily deform fascia, the clients of poorly trained therapists would leave looking like slightly squished clay models. The real changes in fascial stretch therapy come from the guided way that your own muscles affect your connective tissue.
Active/Passive Release and Activation Techniques
In addition, we use a variety of techniques that are similar to what you may see referred to as reciprocal inhibition, positional isometric release, active release and strain-counterstrain. There some similarities between all of them. However, there are important differences that help decide which is the best technique to use.

Vigorous stretching of your neck can cause problems.
In myofascial treatment, we usually passively run the muscles we’re working on through their full pain free range of motion. So, that means that you don’t use the muscle to move it. Either someone does it for you or you use props to minimize active use of the muscle. However, we don’t just gently stretch it. Importantly this means we also shorten the muscle.
We Only Engage In Limited, Gentle Stretching Of The Neck
 There are some gentle stretches for key neck muscles that I might recommend in some cases. However, because of the delicacy of these muscles, you can easily overdo it and make things worse.
There are some gentle stretches for key neck muscles that I might recommend in some cases. However, because of the delicacy of these muscles, you can easily overdo it and make things worse.
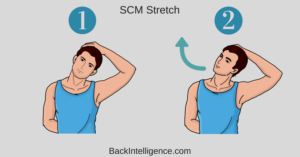
For instance, the sternocleidomastoid (SCM) stretch pictured should be done very gently and only after releasing the muscle. .
In fact, we are quite am conservative about this and more likely to recommend stretches for the chest, upper back and arms than neck stretches for most headache sufferers.
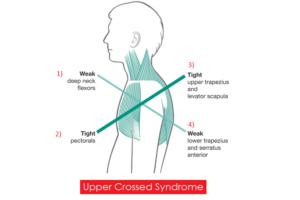
Upper Crossed Syndrome
For many headache sufferers, the myofascial issues are part of a larger pattern of imbalance such as Upper Crossed Syndrome. Re-establishing balance between the postural muscles of the upper back, neck and shoulder is essential. This means that deeper stretching is probably going to be limited to our chest and our upper traps/levator scapula. Meanwhile, we might try to strengthen the deeper muscles in the front of our neck and our lower traps.
Myofascial and Trigger Point therapists, often recommend simple, gentle exercises to strengthen the deep cervical flexors!
For instance, shorter upper arms might cause you to unconciousously lean-in to your work. This could encourage you to round your shoulders and crane your neck forward.
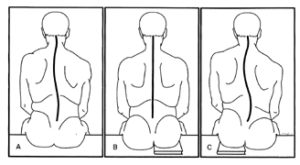
Another common variation is a difference in the size of the two sides of the your pelvis. This can cause you to sit with a tilted base of support. In turn, this may lead to a functional scoliosis that runs all the way up to your head.
Naturally, these types of variations can contribute to headaches. However, even variations in the structure of your foot can lead to headache. There is a well documented referral from the soleus muscle, deep in your calf, to the head.
As myofascial therapists, we routinely look for these variations and encourage effective corrections.
Get Better Sleep, Reduce Chronic Pain
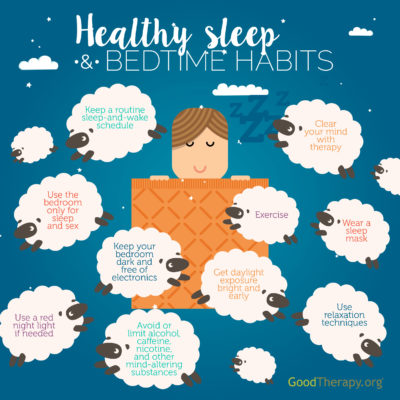
Yes, getting good quality sleep is important!
Sleep is a natural process when we rest and repair ourselves. In fact, a minimum amount of sleep is needed for survival. In addition, we need larger minimum amount of sleep to be at our best.
Ideally, we don’t need to do anything about sleep. We get tired, we go to bed, sleep all night and wake up the next day feel refreshed.
Sadly, sleep often doesn’t go the way we expect. Often, we may be tired when shouldn’t be and unable to fall asleep when we go to bed. Sometimes, we may not sleep through the night. Or, we may sleep enough hours, but not get enough deep sleep. Finally, when we wake up in the morning, for some of us, that is one of the worst times of the day. Now, everything hurts and it takes a significant amount of time to “warm up” and feel better.
First, to get better sleep, we need to do is regulate our schedule.
Set a time to go to bed and get up and stick with it. If you can, the includes weekends.
Also, eating regular meals at consistent times help regulate our systems.
In addition, don’t nap during the day and get adequate sunlight. This helps set your body clock properly.
Avoid habits that interefere with good quality sleep. Make some new good habits. You’ll sleep better!
First, to get better sleep, we need to do is regulate our schedule. Set a time to go to bed and get up and stick with it – even on weekends, if you can. In addition, don’t nap during the day and get adequate sunlight. This helps set your body clock properly.
Avoid habits that interefere with good quality sleep.
Generally, good sleep hygiene is common sense. Most of us already know what do to. But, changing major lifestyle habits is hard. When we realize how far off we’ve gotten from good sleep it can be discouraging.
In that case, consider small steps. Reorganize your bedroom a bit. Focus on reducing just one negative habit and replacing it with one better one.
Rome wasn’t built in a day. One step at a time…
Sleep Posture

Of course, just as when we are awake, some postures are more likely to cause myofacial problems.
Do you sleep on your back, side or stomach? Maybe half-side, half-stomach? But, if on your side, do you curl up? Generally, sleeping flat on your back with little or no pillow is considered natural and ideal.
In fact, this is how infants naturally sleep. However, as older adults, we may find that sleeping on our backs can aggravate low back pain. Also, we are more likely to experience sleep apnea on our back.
So, for for various reasons some of us sleep on our side or stomach. Unfortunately, when we sleep on our stomach our head and neck are turned to one side. Obviously, this causes problems with muscles in head, neck, shoulders and arms.
Sleeping on your stomach is bad. Period.
Often, side sleeping is a great compromise for many people. However, side sleepers need to pay more attention to pillows than people sleeping in other positions. Also, notice the difference for you between ‘half-stomach/half-side” and being purely on your side. True side sleeping means you are laying on your arm OR that you tend to let your shoulder round in. Pillows can help with this.
Most of us sleep with too many pillows, not enough pillows or the wrong kind of pillows. And, this is potent factor is in perpetuating myofascial pain.
Back Sleepers
We recommend a single, very thin pillow under your head. In addition, if you experience low back pain when laying on your back, you may find that bolster under your knees helps. Of course, this could be another ordinary pillow, but a good bolster is round, thick enough and will hold its shape all night.
Side Sleepers
First, we recommend a thick pillow at the head. If you wake up with a hand or arm tucked under your head, that is your body telling you that your pillow is too thin! Side sleeper pillows are either thick and firm OR they have fill that can be positioned as you want it and will mostly keep its shape during sleep.
Next, let’s think about your arms. Naturally, the arm you are sleeping on needs to be accomodated. Try placing a thin pillow under your rib cage. This creates a “slot” for this arm and shoulder. In addition, your upper arm should rest on a thick, firm pillow or bolster. As much as you love your partner, we all need to find a sleeping position that works for us on our own.
Finally, consider your legs. Unfortunately, flexing the hips and/or knees and curling up close to a fetal position is hard on our hip flexors and hamstrings. Try to avoid this. A thick, firm pillow or bolster should be used in between the lower legs. Remember, the idea is to keep your knees and ankles about the same distance apart as your hips.
Avoid foam…
First, we do not recommend foam pillows of any type. Even if you are happy with your foam mattress, we don’t recommend foam pillows. They do not maintain their thickness. In addition, they ‘jiggle’ which is not good for your neck. Of course, it you have any concerns about the foam material itself, you don’t want it near your nose and mouth all night. Besides, there are a variety of other materials that are better for conventional head pillows.
Next, there are a variety of side sleeper pillows in various shapes, including ‘L’ and ‘J’ shaped. For those who go back and forth between back and side sleeping, consider the “Tri-Core” pillow or similar.
Basically, thick pillows and bolsters used to support your limbs need to keep their shape all night. They should be made with dense cotton stuffing or similar.
Feet and Ankles
Sometimes, we need to pay attention to foot and ankle positioning at night. For instance, if we have myofascial issues in the calf, we want to avoid pointing out toes. So, back sleepers probably want to use a bolster of some type to help keep their ankles from drooping at night.
In addition, this means that we might not want heavy covers or sheets tucked in at the foot of the bed. They will weigh down our toes and point our feet and ankles.
Sleep Hygiene

When we are in chronic pain-better sleep is more important than ever. There are many things we commonly eat, drink and imbibe in the evenings that can interfere with your sleep. These are common recommendations for good sleep hygiene.2
Substances
- Caffeine – Some people find that it affects them so strongly that coffee, tea, colas or energy drinks after noon can affect sleep.
- Alcohol – Although alcohol is a depressant, and too much will cause you to pass out, alcohol interferes with your sleep architecture. If you enough, but still feel tired in the morning, consider avoiding alc0hol for 3-4 hours before you go to bed.
- Muscle relaxers, opiates, marijuana (w/THC) – Our advice is similar to alcohol. All are best avoided later in the evening. CBD products may be a different story.
- Liquids – It seems obvious right? We knew this as small children. If you consume significant amounts of liquid before bed, it is much more likely that you will need to get up at night to use the bathroom.
Other Factors
- Blue light – Electronic screens from phones to computers to TVs emit a large amount of blue light that can interfere with sleep. Avoid them for as long as possible before sleep.
- Stress – Getting mentally or emotionally involved in something significant can be stressful. Stress increases cortisol levels. However, cortisol promotes daytime energy and interferes with sleep.
- Exercise – Regular aerobic exercise is good in many ways, including for promoting sleep. However, most of us sleep better if we avoid vigorous exercise in the hours immediately before bed.
If you are already avoiding liquids and getting up at night purely to use the bathroom, this is NOT normal. Men should see a urologist about prostate and/or bladder issues. Both men and women should consider gentle self-care for their pelvic floor. Some pelvic floor issues can be treated externally. Internal therapy for pelvic floor issues is controversial and outside of the scope our practice.
If are able, our bedrooms should be for sleeping only. Our bodies and brains learn what to expect based on what we do and where we do it. If we avoid eating, working, studying and watching TV in the bedroom, it helps to program our system correctly.
We understand biologically that when we go to bed and turn out the lights, it is time for sleep. Instead, if we frequently go to bed, turn out the lights and turn on the TV, we have sent a confusing message to our brain.
Temperature
The temperature of your bedroom under your covers and pajamas is important. If it is already bedtime and we are laying down with the lights out, the next cue that our bodies use is temperature. Cooler temperatures encourage sleep. If you wear pajamas make sure you are not too warm.
Your head, hands and feet are all powerful radiators. If you have trouble falling asleep make sure the room is cool (65-70F), you are not wearing socks, your hands are outside of your covers and your head is uncovered. Maintain adequate humidity in the winter (above 25%).
Avoid drafts, especially on your head and neck. This can activate myofascial trigger points in your neck. Do not make the room too cool. If you are cold at night you are more likely to curl up in a fetal position.
Other Conditions In Your Bedroom
If you have blinds or curtains, use them. Keep your bedroom dark when you are sleeping. Try not to have mirrors positioned that can reflect light on you while you sleep. Avoid flashing lights. Clock radios and other appliances with blue lights can especially troublesome.
Couples
Couples need to work out how to handle schedules that are not aligned. If one of you is having sleeping problems, snoring or otherwise disturbing the other, it may require separate sleeping arrangements for a short while.
Some medications that you are taking may interefere with the amount your sleep. Instead, some can make your sleepy but interfere with the quality of your sleep. Be aware of these effects and discuss them with your doctor.
Medications to promote sleep generally fall into two broad categories.
Medications To Fall Asleep
Melatonin – For example, melatonin is a popular, OTC product that helps us fall asleep. Melatonin is actually a naturally occuring hormone in our body that sends a signal to our brain that it is time for sleep. As we sleep, we use up our melatonin and start making cortisol. When we wake up, our melatonin level should be low and our cortisol level high. This gives us the energy to get through the day. By evening, our cortisol level should be dropping and our melatonin level increasing. The exposure of our eyes to light is one of the ways we make melatonin. If we don’t get enough daylight or our schedule is disrupted by shift work, melatonin 30 minutes before bed might help. We also make less melatonin as we age.
Other sleeping aids, from Sominex to Ambien use different mechanisms to help us fall asleep. Like melatonin, they do not help us STAY asleep.
Medications To Stay Asleep
There are various prescription medications to promote deeper sleep. Consult with your physician for more details.
One of the most commonly prescribed is trazodone. Originally developed as an anti-depressant, small doses of trazodone help some people sleep better. Often, it is prescribed for chronic pain patients. Other types of anti-depressants have also been used to improve sleep.
Pain at night can wake you up. For this reason, muscle relaxants and opiate pain medications may be prescribed before bed. However, these medications may interfere with your sleep architecture. Discuss with your doctor what the best time is for you to take these medications.
Good Sleep Matters!
What Else Contributes To Chronic Headaches?
Do These Things To Feel Better!

- Keep a headache diary - Discover more about what triggers or contributes to your headaches and what treatment is most effective.
- Try relaxation techniques - This can teach you ways to deal with stressful situations. This might help reduce the number of headaches you have.
- Improve your posture - Good posture allows your neck muscles to work properly.
Get Organized
- Improve your work furniture - Consider a standing desk. Make sure your work area is arranged to minimize repetitive head and neck movement.
- Increase aerobic exercise - We go beyond this and encourage healthy movement that my include yoga, dancing, Pilates or other classes.
- Firm up your routines - Don't sleep too much or too little. Set and follow a consistent sleeping schedule. Eat nutritious meals at regular times.
- Drink plenty of fluids - Staying properly hydrated will help, but don't over do it. Alcohol and coffee are dehydrating.
- See The Eye Doctor Regularly - Poorly fitting eyeglasses or improper prescriptions can contribute to headaches. Discuss pros and cons of progressives versus two pairs of glasses, monovision or other approaches.
Coping and support
Living with chronic headaches can be frightening and difficult. The attacks can seem unbearable and make you feel anxious and depressed. Ultimately, they can affect your relationships, your work and the quality of your life. Talking to a counselor or therapist might help you cope with the effects of chronic headaches. And, joining a headache support group can connect you with others. The may have similar experiences and share helpful information.You can do this!
Avoid These Things!

- Stress.
- Smoking.
- Dehydration.
- Excess alcohol.
- Clenching/bruxism.
- Head forward posture.
- Improper (chest) breathing.
- Rebound from caffeine and other medications.