Of course, there are many kinds of pain and different causes. Yet, most types of chronic pain share a similar pattern:
- Initially, some form of local pain happens.
- Then, pain recurs. Your nervous system gets sensitized.
- Eventually, your threshold lowers for local pain.
- Finally, additional stresses ramp up the runaway pain cycle…and we may end up disabled by pain that isn’t even there!
This process applies to many types of pain. Examples include, chronic headache, low back pain and fibromyalgia. There are many treatments available, but effectiveness varies. Fortunately myofascial therapy uses a range of safe and effective treatments to reduce chronic pain.
Put a myofascial therapist on your team!
Chronic Pain Characteristics
- Primary pain: 3 months of persistent pain in one or more areas.
- Cancer pain: from cancer or treatment related pain.
- Posttraumatic pain: 3 months post trauma or surgery.
- Neuropathic pain: caused by damage to the sensory nervous system.
- Chronic headache and orofacial pain: originates in the head or face for 50% or more days over a 3 month period.
- Visceral pain: originates in an internal organ.
- Musculoskeletal pain: originates in the bones, muscles, joints or connective tissue.
Examples
Chronic Pain Prevalence Surveys
A large-scale telephone survey of 15 European countries and Israel was conducted. 19% of respondents over 18 years of age suffered pain for more than 6 months. This included the last month, and more than twice in the last week. Their pain intensity was 5 or more for the last episode. 4,839 of these respondents with chronic pain were interviewed in depth. 66% scored their pain intensity at moderate (5–7), and 34% at severe (8–10). Further, 46% had constant pain and 56% were intermittent. 49% had suffered pain for 2–15 years. In addition, 21% had been diagnosed with depression due to the pain. 61% were less able to work outside the home. 19% had lost a job, and 13% had changed jobs due to their pain.6Prevalence in the United States
In the United States, the prevalence is estimated to be approximately 35%. In fact, approximately 50 million Americans experience partial or total disability.7 According to the Institute of Medicine, there are about 116 million Americans living with chronic pain. This suggests that about half of American adults have some chronic pain condition Journal of the 8. In an internet study, prevalence was calculated to be 30.7% of the population. This broke down to 34.3% for women and 26.7% for men.9.Developed vs Less Developed Countries
Notably, prevalence of chronic pain is generally higher in more developed countries. It is higher still for the US. Possibly, this is something of a "first world problem". Also, it may be under-reported in other cultures. Perhaps few people are even asking people about their pain. Possibly, it could be that other cultures offer different forms of treatment that are effective. On the other hand, simpler life-styles with less stress might promote healing.The impact of chronic pain on cognition is under-researched. However, several tentative conclusions have been published. For instance, most people with chronic pain complain of some cognitive impairment. This includes forgetfulness, difficulty with attention, and difficulty completing tasks.
Objective testing has found chronic pain sufferers experience a wide range impairments. This includes:
- Attention.
- Memory.
- Mental flexibility.
- Verbal ability.
- Speed in cognitive tasks.
- Speed in executing structured tasks.10
How Do Simple Pains Become Chronic?
Chronic Pain Characteristics
For instance, before low back pain becomes chronic, we have a particular injury. Maybe we have occasional episodes. Maybe, it’s just a trigger point in a muscle. It might even be a disc injury. But it will heal.
The same thing happens with a headache. Occasionally, muscular problems or swollen blood vessel might cause a headache. They pass.
Over time, the pain of an injury should subside. However, if it doesn’t we might think our back problem is getting worse. Often, we also won’t be able to detect any deterioration. In fact, an MRI might even show improvement.
So, if our back has healed but our pain has actually gotten worse, what is going on?
Unfortunately, we may have developed central sensitivity to this local pain. Now, imagine that you have central sensitivity AND the local pain continues.
Ultimately, this is how severe chronic pain develops.
Chronic Pain and Central Sensitivity

Allodynia
Allodynia occurs when you experience pain from things that are normally not painful. For example, simple touch or pressure become painful. Nerves in the area touched send signals to your brain. But, your nervous system is in a heightened state. So, your brain doesn't produce the mild sensation of touch it should. Instead, it produces pain and discomfort.Hyperalgesia
Hyperalgesia occurs when something painful is more painful than it should be. For example, a simple bump would ordinarily be mildly painful. However, if you are a chronic pain patient it might send your through the roof. Again, your nervous system is more sensitive. Of course, it produces pain that is amplified.Other Symptoms of Central Sensitization
Central sensitivity has other characteristics. They occur less often. For example, it can lead to heightened sensitivities across all your senses. For instance, some chronic pain patients report sensitivities to light, sounds and odors. Normal levels of light can seem too bright. Perfume can produce a headache...12 In addition, central sensitivity may cause cognitive deficits. For instance, this includes poor concentration and poor short-term memory. Also, it corresponds with increased levels of emotional distress, particularly anxiety. After all, the nervous system isn't just responsible for sensations, like pain. In addition, it produces our emotions.13 Central sensitivity can occur with chronic low back pain, chronic neck pain, whiplash injuries, headaches and more.14Fortunately, for Chronic Pain - Myofascial Trigger Point Therapy helps break the cycle...
Local Causes
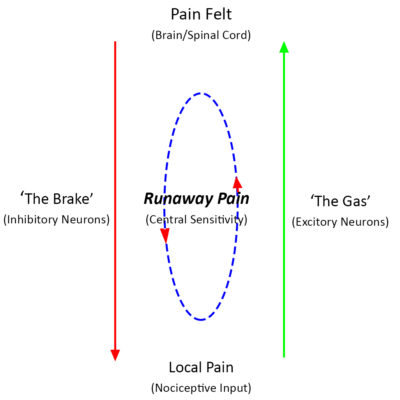
Chronic pain begins with a Local Pain or peripheral issue of some type.15 For instance, it could be an injury or surgery. Sometimes it is myofascial pain or trigger points. In a migraines, it could include pain from swelling blood vessels. Instead, in a low back pain, it could be compression of a nerve root.
In fact, the nature of the initial pain can vary greatly. Initially, the ‘Pain Felt’ is proportional to the cause.
However, if the pain is severe/and or recurs, our perception of it can change and the Pain Felt grows out of proportion.
Transition to Chronic Pain
Eventually, our recurring local pain transforms into Centralized Pain. In some cases, our pain “Brake” doesn’t work. This can lead to the all-over sensitivity of fibromyalgia. For others, our pain “Gas pedal” is stuck on. This can lead to multiple discrete painful areas without a reasonable cause. This is called Myofascial Pain Syndrome.16
Either way, we can see that less brake or more gas will feed the Runaway Pain loop. This makes another episode of Pain Felt more likely and more severe. Ultimately, this results in the transition of your episodic pain into chronic pain.
Once we have developed this type of chronic pain, many things can mess up our Brakes and Gas even more. Poor sleep interferes with your Brakes. Stress pours on the Gas.
Getting Better
Treatments that improve your Brakes and cut back on the Gas slow down the Runaway Pain loop. This will reduce our pain.
Fortunately, if you have chronic pain – myofascial trigger point therapy works!
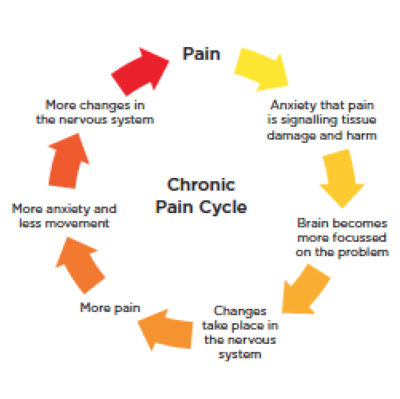
Typically, if your pain lasts longer than six months, it’s considered chronic pain. Sometimes, pain causes other complications. These complications, in turn, can make the pain worse. A chronic pain syndrome is a vicious cycle of chronic pain and the secondary complications, making the pain worse. What are these secondary complications?
Poor Sleep
Chronic pain can lead to some common problems over time. For example, many people tend to have trouble sleeping because of pain. Then, your body doesn’t repair properly during sleep. Eventually, you may be so tired that everything starts bugging you. Also, coping your pain gets harder too.
Some people stop working. Then, they might come to experience financial problems. Often, the stress of these problems keeps them up at night. Of course, thinking too much at night can make your sleeping problem even worse.
Social and Emotional Stress
Chronic pain can also affect the roles people have in the family. For instance, you may miss out on children’s activities, family functions, and parties with friends. As a result, many people struggle with guilt.
Unfortunately, guilt isn’t the only negative emotion associated with chronic pain. Typically, you might experience a combination of fear, irritability, anxiety and depression. In addition, they may also express a lack of direction.
Centralization
These problems are called stressors. This means that they are problems that cause stress. And, stressors can make pain worse because stress affects the nervous system. It makes the central nervous system more reactive. Then, these stressors combine with the initial pain to create central sensivity. Unfortunately, this magnifies everything and reinforces the cycle..
The vicious cycle of pain becomes clear. Chronic pain causes stressful problems. These in turn, cause stress that makes your pain worse. Finally, this combination of initial pain, other stressors and central sensitivity causes a chronic pain syndrome. There are many fancy terms for this. However, we refer to this pain as ‘centrally mediated’. This is because your central nervous system mediates your peripheral or other local pain poorly.17
Typically, severe chronic pain comes from a failure of effective central mediation…
Psychological Aspects of Chronic Pain

Some researchers believe that individual psychology is significant. It may help us understand why some develop chronic pain and another doesn’t.18
Personality Types
There are two distinct personality types that are common in chronic pain patients. First, is a type with exaggerated concern over body feelings. They develop bodily symptoms in response to stress. Often, they fail to recognize their own emotional state. They may be depressed.
On the other hand, the ‘neurotic triad’ personality also expresses concern over body feelings. In addition, they develop symptoms in response to stress. However, they tend to be demanding and complaining.21 Self-esteem also shows striking improvement once pain has resolved.22

Social support has important consequences if you have chronic pain. In particular, consider pain intensity, pain control, and resiliency to pain. They are all influenced by different levels of social support.
People with persistent pain conditions tend to rely on their social support as a coping mechanism. Therefore, they have better outcomes when they are a part of more supportive social networks.
There is a direct significant association between social activities or social support and pain. Higher levels of pain were associated with a decrease in social activities. In addition, it correlates with lower levels of social support and reduced social functioning.23
Catastrophizing may play a role in chronic pain. Pain catastrophizing is describing pain in exaggerated terms. We may think a lot more about the pain when it occurs. Lastly, we may feel more helpless about the experience.24
People who score highly on these measures are likely to rate pain as more intense. Previously it was thought the tendency to catastrophize causes this. The person experiences the pain as more intense. Maybe, they had altered anticipation and emotional responses to pain.25
Again, some aspects of catastrophization may be the product of intense pain, rather than its cause.
That is, the more intense the pain feels, the more likely one is to have catastrophic thoughts.26
What Are The Treatment Options?
"There are both oral and topical medications. Oral medications include nonsteroidal anti-inflammatory drugs, acetaminophen, and opioids. Topical ointments or patches are applied to the skin. We place some of these patches on top of the painful area. Then, the active drug, such as lidocaine, is released. Others, such as fentanyl patches, may be placed at various locations. Some medications require a prescription.
"Finally, there injections into various levels of the spinal region. For example, trigger point injections are made directly into painful muscles. Some injections involve more invasive procedures. Epidural injections are done for pain the neck/arm and back/leg. In addition, facet injections are done into the spinal facet joints. These allow you to move your neck and back. There are also injections for burning pain of the arms or legs from Complex Regional Pain Syndrome or Reflex Sympathetic Dystrophy (CRPS)."
What are these medications? What are some of the common side effects ?
In general, your primary physician or pharmacist may be to answer any questions about the action, dosage and side effects from these medications. For convenience, we divide commonly used medications into these broad categories:- Nonsteroidal Anti-inflammatory Drugs and Acetaminophen: NSAIDs can be very effective for acute muscular and bone pain as well as some types of chronic pain syndromes. When taken for an extended period of time or in large quantities, they may have negative effects on the kidneys, clotting of blood, and gastrointestinal system. Bleeding ulcers is a risk of these medications. Long-term use of may be associated with an increase in cardiovascular heart risks.
- Muscle Relaxants: These medications are most effective for acute muscle spasms in chronic pain patients.
- Opioids: When used appropriately, opioids can be very effective for some types of pain. They tend to be less effective or require higher doses in nerve type pain. Usually, with constant severe pain, a long acting opioid is recommended. One of the most frequent side effects is constipation. In addition, they can cause drowsiness which often gets better over time. Nausea is another side effect which may be difficult to treat and may require changing to another opioid.
What About Nerve Blocks?
Nerve blocks have a role primarily in the reducing the input of severe pain stimulus to your nervous system. That means that if your chronic pain is at least partly because of inflammation of a specific nerve or nerve root, a steriod or anesthetic block may provide temporary relief. These can help break the cycle of chronic pain but will not cure it. Most nerve block injections done on an outpatient basis. All of them may be performed under x-ray guidance. However, sometimes they are performed in the office without x-ray. Below is a brief description of some common nerve blocks:- Epidural Steroid injection: This an injection performed in the back or neck. It is an attempt to place some anti-inflammatory steroid close to the inflamed area causing the pain. Generally, these injections are done for pain in the back/leg or the neck/arm. They may be done under x-ray guidance.
- Facet Joint Injection: The facet joints assist with movement of the spine both in the neck and back. Injection into these joints can provide relief of neck and back pain. These injections are always performed under x-ray guidance. A needle is placed in your neck or back and advanced in the joint under x-ray visualization. Contrast dye is used if the needle is put within the joint. Sometimes, it is also used if the injection is designed to numb the nerves to the joint. This block is often a diagnostic block. If you have significant pain relief from this injection, a more long lasting injection may done.
- Specific nerve blocks: The pain of occipital neuralgia, for instance, can be excruciating and can become chronic. Although there may be myofascial factors underlying that pain, an anesthetic block of the occiptal nerve can provide, immediate, but temporary relief.
Nerve Blocks for Chronic Regional Pain Syndrome
- Lumbar Sympathetic Block: A lumbar sympathetic nerve block is performed for pain in the leg of CRSP type I. Local anesthetic is placed near to the lumbar sympathetic chain in order to relieve the pain. Your leg will likely become warm immediately following the injection. However, this is an expected effect and not a complication. If it is done under x-ray, a small amount of dye is injected. This makes sure the needle is in the right spot. The the doctor will inject numbing medicine and remove the needle.
- Stellate Ganglion Block: A stellate ganglion block is an injection for diagnosis of CRPS of the arm or hand. It is also used for treatment of pain to that area. In some cases, it can also be used to help to improve blood flow to the hand or arm. This injection is performed with or without x-ray guidance.