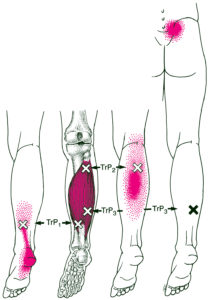
Sorting out lower leg pain? Trigger point referrals are usually pretty straightforward. First, we divide your leg into three sections, the front (your shin), the outside, and the back (calf).
Each of these sections has a small number of muscles that cause myofascial pain. Quickly checking the referral patterns of these muscles helps us zero in on some likely targets.
We’re most likely to find problems with the tibialis anterior (TibA) muscle. This most common in runners and other athletes. Many of us have also experienced pain in this area as “shin splints” after unusual exertion.
We could also find trouble well up the inner thigh, with your adductors. They refer down the inside/front of your leg to the ankle.
The combination of the soleus and gastrocnemius (gastroc) make up the bulk of our calf. These are the muscles that provide power in our lower legs. However, your soleus works harder and is more likely to cause you pain.
We can also get referrals down the back of the leg from the gluteus minimus (glute min), deep in our hip.
Lastly, we access the tibialis posterior (TibP) muscle from the inside, but its referral pattern is towards the back.
Check the links above to other pages for pain this area…
Typically, we are most likely to get pain from our gastroc on the outside of our leg.
However, as with the back of your leg, you can get referrals down the outside of your leg. They come from the gluteus minimus (glute min), deep in our hip.
Sometimes, we get pain from the fibularis longus and brevis muscles.
Lower Leg Pain – Trigger Point Referrals
Our gastroc (gastrocnemius) is the large muscle in our calf that gives it shape. When we wear high heels, it shortens and becomes even more shapely. However, as we see later, beauty comes at a price. Our gastrocnemius (gastroc) muscle works hard. Usually, it doesn’t give us much trouble. But when it does, it gets our attention!
Our gastroc has a “reverse pull” arrangement. That means that the smaller part (our leg) pulls on the more substantial part (our bodies).
 As we walk, it uses lengthening contractions most of the time. It works with other plantar flexors to resist the rotation of our lower leg over our ankle. Of course, when our foot is free, the primary function of our gastroc is to plantarflex, or ‘point’ our foot.
As we walk, it uses lengthening contractions most of the time. It works with other plantar flexors to resist the rotation of our lower leg over our ankle. Of course, when our foot is free, the primary function of our gastroc is to plantarflex, or ‘point’ our foot.
Primary Actions of Gastroc and Soleus
We assume that such large muscles are essential for walking and running. However, the gastroc does not contribute to push-off when we walk or run. Instead, its primary action, whether we are standing, walking, or running, is to stabilize our knee and ankle. It is most active just after heel strike; our knee was previously extended and is just starting to bend. Therefore, controlling this bend is when we see the most activity in our gastroc.
Most often, we activate trigger points in the gastroc with overload or wrong foot position. For instance, you can do this climbing steep hills (or Stairmaster workouts), running uphill, or riding a bike with the seat too low. Any activity where we are forcefully plantarflexing with our knee bent can do it.
Activations From Holding Fixed Positions
Activations can also happen if we leave our foot/ankle pointed too long. For example, long drives with our foot on the accelerator shorten our gastroc. If you keep any muscle in a short position for an extended time it can cause trigger points.
Sometimes, we also develop trigger points in our soleus, which is a helper for the gastroc. Also, we can get them in the muscles that oppose our gastroc. These include our tibialis posterior, toe flexors, and hamstrings.
We know that wearing high heels or driving without cruise control and our foot pointed can cause problems. But, we might not have thought about whether our desk chair is too high. Your feet should fully touch the floor. Otherwise, your foot points, your gastroc shortens, and trouble is brewing.
Avoiding Passive Activations
Or, you might find this happens at night. If you sleep on your stomach, your feet and ankles point. Also, if you sleep on your back with a tight top sheet or heavy comforter, it points your feet. If you have calf cramps at night, this could be a cause. For some, vitamin E is also helpful for calf cramps at night.
Pressure on our gastroc causes myofascial trigger points. Also, tight socks or joint stabilizing sleeves around your ankle, calf, or knee can do this. Restricted circulation causes trigger points and calf pain. Sometimes, the front edge of a chair seat compresses our thigh. This edge can easily restrict blood return. Worse, it can restrict arterial flow. On the other hand, many recliners do not support our feet. The weight of our legs rests on our calf muscles.
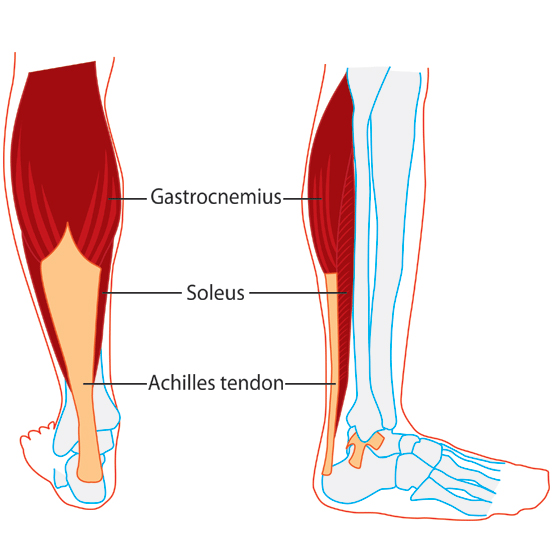
Our soleus (soleus) is the deep muscle in our calf that provides power when running and jumping.
Our soleus spans both bones in the leg at the top. It runs deep in the leg, under the gastroc. Soleus provides some of the bulk in the middle of your calf. Then it gets narrow as it converges with your gastroc to form the Achilles tendon.
The most common trigger points in the body are in our soleus!
Like our gastroc, soleus stabilizes our knee and ankle as we walk. However, when we run, our soleus acts as a significant venous pump. It powerfully returns blood from your legs to your heart. Often, the soleus is called the “runner’s heart.”
Also, our soleus works with our gastroc, fibularis muscles, toe flexors, and tibialis posterior to plantarflex our foot. We oppose this action with our tibialis anterior, toe extensors, and the fibularis tertius muscle. Collectively, these muscles are dorsiflexors. The combination of our soleus and gastroc is much stronger than these dorsiflexors.
Our soleus isn’t very active when we are walking. However, we get a little more power from soleus than from our gastroc when running.
Our soleus contains a large percentage of slow-twitch fibers. That is one of the reasons why it is so resistant to fatigue. Humans can run longer and farther than any other mammals.
Our soleus is one reason why!
Most often, we activate trigger points in our soleus from running and jogging.
 There is vigorous activity in our soleus when we fall. So it is not surprising that falls can activate it.
There is vigorous activity in our soleus when we fall. So it is not surprising that falls can activate it.
We can also activate our soleus while walking in shoes with smooth soles on a slippery surface, walking an incline, or walking in sand.
Don’t wear slippery shoes or high heels. Of course, we know that extended drives without cruise control leads to trouble.
Your feet should fully touch the floor at your desk. If they do not, consider getting an inexpensive footrest. If you have a stand-up desk with a high desk chair, avoid hooking your heel on the rail at the bottom.
 Like our gastroc, shortening our soleus at night causes trigger points. If you sleep on your stomach, your feet and ankles point. Also, if you sleep on your back with a tight top sheet or heavy comforter, it points your feet.
Like our gastroc, shortening our soleus at night causes trigger points. If you sleep on your stomach, your feet and ankles point. Also, if you sleep on your back with a tight top sheet or heavy comforter, it points your feet.
When relaxing in a chair, leg rests and recliners should support both your heels and your legs.
Lower Leg Pain – Trigger Point Therapy
We focus on history, lifestyle, pain patterns and other symptoms to sort out your myofascial pain. There is a myofascial component to many types of stubborn pain.
Notably, myofascial pain is not caused by contracted or ‘tense’ muscles. They have no electrical activity.
Lower Leg Pain – Trigger Point Referral Patterns
We can clearly see how referral patterns of lower legs evoke common pains Some of the factors that activate those muscles may not covered by doctors. Those activation factors are things we care a lot about.
Myofascial activations are a part of most chronic pain!
Repetitive Use
When ever we are making repetitive movements, we should be mind of using proper body mechanics. This will help minimize repetitive stress injuries and myofascial activations. For instance, lifting in a stooped posture and then twisting is always ill-advised. Doing it repetitively is worse. Therefore, if this type of lifting is required, we should rethink the task and try to organize it in a way that reduces stooping and twisting. However, even simple movements matter. For instance, what if your desk is arranged phone on the wrong side. In fact, with every call, you have to twist your head and neck and reach over with your arm to the wrong side of the desk This is poor body mechanics. Fixing it might be as simple as moving the phone. It pays to think about basic body mechanics in this common sense way each time we engage in a repetitive activity. Fortunately, we're starting to teach this important skill to young people, as in this student guide at University of Michigan.Overload
We can experience chronic overload when we do things like wear high heels, carry a heavy bag or lean into our work. However, acute overload happens when we decide to lift, push, pull or otherwise move something that is too heavy for us. Most often, we overload our muacles with an eccentric contraction. For example, lifting a heavy box, correctly using your legs instead of your back, requires concentric contractions of your quads. However, setting that same heavy box down, slowly and with control, require eccentric, lengthening contractions. These should be done carefully.Spill it!
Of course, if you have a diagnosis from your doctor, we need to know. If you have recent imaging or other test results, even better! We've all been knocked around a bit. We'd like to know everything you can think of about prior accidents, injuries, surgeries and other treatments. It is important to know about previous or current medical conditions that could impact our treatment. Anything from high blood pressure to TMJD to disc problems are vital information. Hopefully, medications align with your diagnosis. Sometimes, certain medications will also modify our reatment options. Some drugs interfere with nutrient absorbtion. Increasingly, supplement use is common and we'll review that with you as well.Lower Leg Pain – Trigger Point Referrals Can Overlap
Although we are focused on the gastroc and soleus, the referral patterns of other muscles are similar. For us to determine which muscle(s) are involved, we need to consider some other factors.
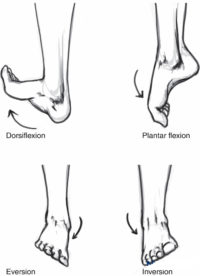 For instance, we consider your range of motion in all four primary directions at your ankle:
For instance, we consider your range of motion in all four primary directions at your ankle:
- Plantar flexion
- Dorsiflexion
- Inversion/Pronation
- Eversion/Supination
Where Does The Pain Refer?
For example, if we want to distinguish between our gastroc, pictured previously, and our soleus, pictured here. They are quite different. Gastroc trigger points cause pain that is mostly in the back of our calf. Soleus trigger points can range from our heel to our sacrum!
Even for pain in our calf, we can see that our soleus is more likely to hurt right in the center. Gastroc referrals tend to be on one side or the other.
Lower Leg Pain – trigger points can be relieved easily with myotherapy.
Aside from referral patterns, we will consider range of motion and your history. Some of the things that activate trigger points in the gastroc and soleus are the same. But some are different. For instance, if your calf pain began after a slip on the ice, we’re definitely taking a look at your soleus before your gastroc!
Determining which muscles are referring pain is crucial to myofascial trigger point treatment…

From the outset, education is important. It is our job as therapists to educate you about our assessment and our process. Then, throughout our treatment, we continue this education process.
Trigger Point Therapy can get at some aspects of myofascial pain that you might not have thought of!
Diaphragmatic breathing is at the foundation of myofascial trigger point treatment. But, if you don’t know how to do it, we will teach you. On the other hand, if you already know about it, we will help you deepen the technique.
Of course, the medications and supplements you are taking matter too. Typically, reducing drug consumption is a good thing. However, it should be done gradually and in consultation with your physician.
Unfortunately, sleep posture and sleep disturbances contribute to many myofascial pain syndromes. However, this is especially important for relief from chronic pain. Because of this, we always have a thorough discussion about how you sleep during an initial assessment.
Structural variations need to be explored and understood. Once treatment begins, they can be accomodated or corrected in various ways.
It is surprising, but most of us our not taught proper body mechanics. Whether we are at home or at work, we need to learn how to use our body correctly.
Most people are self-conscious about their posture. And, posture includes more than how you sit or stand. But, identifying the postural aspects that should be improved is a challenge. Even harder, is understanding how they vary with movement. Ultimately, devising a strategy for improving them is essential.

However, it usually takes more than hands on work to really erase the pain and keep it away.
First, the chances are that we were not your first stop. As a general rule of thumb, the longer you have experienced pain, the longer it will take to make them go away.
Secondly, there are usually at least some factors that affect your pain that we can’t easily change. However, we can usually find the most important factors and devise a strategy together.
Myofascial tigger point therapy – it’s how you work this!
Education is the first step in the myofascial treatment protocol.
Sometimes, we may not be good enough at explaining how myofascial pain works and how it activates your pain.
However, we believe that people can make more progress when they know more about their condition. So, we try to understand what your learning style is give you as much information as you want – but hopefully not too much!
Typically, we performing series of miniature cycles of test/assess, treat and test/assess again. It is an informed exploration for both of us.
We have an initial assessment from your history, postural and range of motion exams, etc. Then, we use various treatment techniques before testing and assessing again.
Manual Therapy Techniques
First, we specifically expertly use manual pressure release therapy, neuromuscular techniques, and deep stroking, friction, skin rolling. When indicated, we also use fascial stretching. Sometimes, we use less common techniques like cupping, spray and stretch and acoustic compression.
Muscle Activation
In addition, we may also use active and passive muscle activation techniques. This includes reciprocal inhibition, postisometric relaxation, contract/relax, strain/counter-strain and muscle energy techniques. Sometimes, we also use hot/cold therapy.
Range of Motion/Testing
Finally, routinely run the muscle we are treating through its entire, pain-free range of motion. This is part of your treatment. However, it also the start of a new test/assess cycle.
We learn together whether your range of motion has increased and whether your pain is reduced. We may have you get up and use your body in the way that causes pain to ‘test’ more dynamically.
As we finish our hand-on work, we transition into learning new movement strategies and self-care.
Myofascial tigger point therapy – it’s how you work this!

Lower Leg Pain Trigger Point Compression – Gastroc and Soleus
Once we have identified some causes of our lower leg trigger points, we can focus on other aspects of self-care.
We recommend a roller like the Tiger Tail to locate and compress trigger points in the gastroc and soleus. Less is more. We want to use just enough compression to release a trigger point. More is not better. It is likely to inflame your muscles further.
Myofascial self-care helps reduce the frequency and severity of pain!
Lower Leg Pain – Trigger Point Therapy Stretches – Gastroc and Soleus
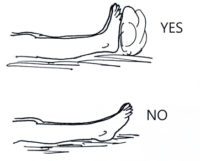
 Most of us know a basic standing calf stretch for the gastroc.
Most of us know a basic standing calf stretch for the gastroc.
Make sure to keep the feet pointed straight ahead during this stretch. If your foot is externally rotated, that ‘cheats’ the stretch. Then, you get less benefit.
 However, we can see that the stretch for the soleus is a little different. You should have the knee of the leg you are stretching bent in a soleus stretch. Both feet should still point forward.
However, we can see that the stretch for the soleus is a little different. You should have the knee of the leg you are stretching bent in a soleus stretch. Both feet should still point forward.
We can also stretch our gastroc and soleus in yoga poses such a Warrior I and Downward Facing Dog. The same rules about straight and bent knees apply. A downward dog with straight knees stretches your gastroc. With bent knees, if stretches your soleus.